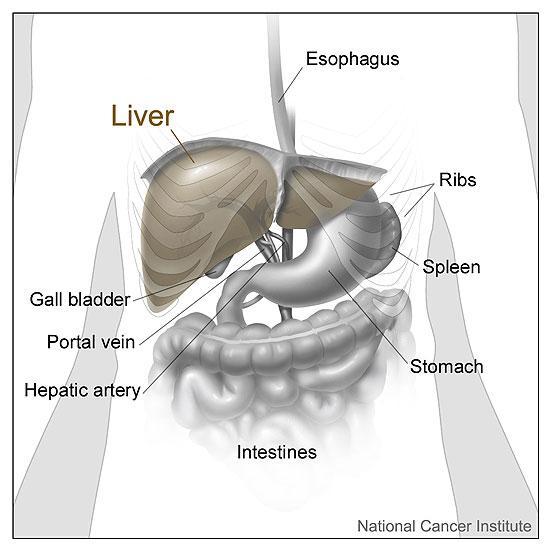
To screen for and monitor liver disease
Liver Blood Tests
When you have symptoms of a liver disorder such as jaundice or have been exposed to substances that can cause liver damage such as a paracetamol overdose, or routine monitoring of many medications
A blood sample taken from a vein in your arm
None
-
How is it used?
Liver blood tests are used to help determine the cause of symptoms such as jaundice that may be due to liver disease. They are also used to screen for potential liver damage, for example in problem drinkers or people exposed to the hepatitis virus, and also to monitor changes if liver blood tests are abnormal.
-
When is it requested?
These tests are used when symptoms suspicious of a liver condition are noticed. These include: jaundice, dark urine and light-coloured stools; nausea, vomiting and diarrhoea; loss of appetite; vomiting of blood; bloody or black stools; swelling or pain in the belly; unusual weight change; and fatigue or loss of stamina. One or more of these tests may be requested when a person has been or may have been exposed to a hepatitis virus; has a family history of liver disease; has excessive alcohol intake; or is taking a drug that can cause liver damage.
-
What does the test result mean?
It is important to note that abnormal results in the individual tests can occur in conditions that do not involve the liver or the bile ducts and that, conversely, normal results can be found in patients with serious liver disease. However, one or more abnormal liver blood test results often point to a diagnosis or to further investigations.
- Raised alanine aminotransferase (ALT) and aspartate aminotransferase (AST) values indicate leakage from cells due to inflammation or cell death. Liver disease is more likely when the values of AST and ALT are higher, ALT rising more than AST in acute liver damage such as hepatitis. When there is doubt about the source of the high enzyme levels, a raised creatine kinase (CK) would suggest muscle damage and measurement of troponin will show whether it is the heart that is damaged. Gamma-glutamyl transferase (GGT) can be more sensitive than ALT and AST for detecting liver damage from drugs, obesity and alcohol, and for detecting early rejection after liver transplantation.
- A raised total bilirubin is usually due to liver disease or blockage of the passage of bile to the gut, for example by gall stones. Bilirubin is made water soluble (conjugated) by the liver and is then excreted in the urine, the stools becoming pale. However, a raised bilirubin can also occur in conditions where the breakdown of red blood cells produces more unconjugated bilirubin than the liver can handle, for example in newborn babies and conditions of abnormal haemoglobin like sickle cell anaemia. If this is suspected, both total and conjugated bilirubin are measured and monitored.
- Liver disease and blockage of the bile ducts also increase alkaline phosphatase (ALP). This is believed to be due to increased bile duct pressure causing the liver to make more ALP. If there are localised lesions within the liver, for example deposits of cancer cells, then ALP may be stimulated to rise but there may be sufficient normal liver around the deposits to keep bilirubin normal. Bone disease can also increase ALP, for an example fracture or vitamin D deficiency. In patients with a normal bilirubin and a raised ALP, the measurement of gamma-glutamyl transferase (GGT) can help. It tends to rise with liver ALP but is normal in bone disease.
- Albumin is made only in the liver and may be low when there has been extensive loss of liver tissue in long-standing disease. Other causes of a low albumin include malnutrition (which may accompany alcoholic liver disease), kidney disease, due to loss of protein in the urine, and inflammatory conditions anywhere in the body.
- Total protein is usually normal in liver disease. The difference between its concentration and that of albumin, called globulin, tends to increase when albumin falls, but very high values are seen most commonly in alcoholic hepatitis and in hepatitis caused by the body producing antibodies against its own liver (autoimmune hepatitis).
- Patients with liver disease often bruise easily and cuts take a long time to stop bleeding. A long prothrombin time (PT) suggests a deficiency of clotting factors made by the liver or a deficiency of vitamin K which is needed for the factors to work. The deficiency can be the result of severe malnutrition, for example in alcoholism, or the result of blockage of bile passage to the gut. (Bile contains bile salts that are needed for the gut to absorb fat, and vitamin K is fat soluble.) Patients with a long PT may be given an injection of vitamin K and the PT measured again in 24 hours. A quicker PT after the injection indicates a deficiency of vitamin K rather than of clotting factors.
-
Is there anything else I should know?
Depending on the history, examination and results of the liver blood tests your doctor may request one or more further tests including hepatitis virus antibodies A, B and C, alpha-fetoprotein (AFP), alpha-1 antitrypsin (mostly for children), copper, caeruloplasmin, iron and transferrin and smooth muscle antibody. Sometimes imaging scans are requested.
-
Why does my doctor want to know what medicines I am taking?
-
Can I have liver disease if I feel fine?
-
Can I have abnormal test results and not have liver disease?
-
Why is my family history important?
Some liver conditions may be inherited, such as haemochromatosis, Wilson's disease and alpha-1 antitrypsin deficiency. Early detection of these conditions allows them to be treated and managed appropriately.