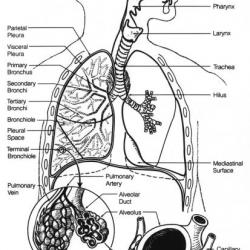
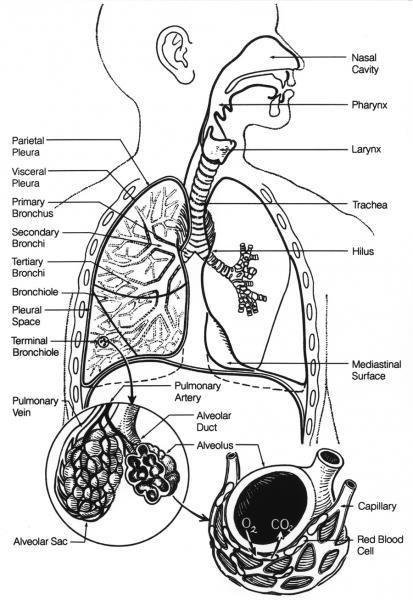
Lung diseases can affect all parts of the lung. In some cases the alveoli are damaged and this impairs the transfer of gases from the air sacs (alveoli) to the blood (and vice versa). In other cases the problem is that not enough air gets to the air sacs. This could be due to blockages in the bronchial tree or weakness in the muscles that expand the chest. In some cases the lungs struggle to remove or detoxify dangerous substances – this could be due to problems with mucus such as cystic fibrosis or due to overwhelming toxins such as smoking.
Common Lung diseases include:
Asthma is a lung disease where inflammation of the bronchi and bronchioles prevent enough air getting to the air sacs. Asthma often happens as an attack which can be triggered by many things. Triggers can include:
-
cigarette smoke
-
moulds and pollens
-
infections
-
exercise
-
cold air
During an attack, the lining of the airways swell and the muscles surrounding the bronchi contract, narrowing the airway. Mucus secretion lining the airways increases and this can slow the movement of air making breathing difficult. All these mechanisms contribute to causing a narrowing of the airways and this often causes a wheezing sound. Most episodes do not cause long-term lung damage but it is often necessary to see a doctor since lack of oxygen and build-up of carbon dioxide can be life-threatening. Patients use inhalers to help open up the airways. According to Asthma UK, 1 in 5 households in the UK have a person with asthma.
COPD ( obstructive pulmonary disease) is a term used for both and chronic bronchitis. With chronic bronchitis, the bronchial tubes become inflamed and scarred. This reduces air flow within the lungs and can result in more mucus production. With emphysema, the air sacs in the lungs are slowly destroyed. The combination of these changes often results in the typical symptoms of cough, shortness of breath and increased sputum production that is found with COPD. Patients with COPD find it hard to breathe and have long term problems getting enough oxygen to the blood and carbon dioxide out due to the damage to the air sacs and the narrowing of the airways. The main cause of COPD is smoking. Other risk factors include repeated exposure to air pollution fumes, dust and genetic disorders, but these are rare. It is estimated that COPD causes around 25,000 deaths a year in the UK.
Pneumonia is a complicated inflammation of the lungs usually caused by or a. This infection and inflammation causes the small air sacs of the lungs to fill up with fluid impairing the exchange of gases. Pneumonia can affect one area of a lung or both lungs (bilateral). A patient may cough up sputum, have a fever, and feel tired. Doctors can sometimes hear signs of pneumonia when listening with a stethoscope. X-rays can help by showing areas of inflammation (consolidation). Antibiotics are used to treat bacterial pneumonia. The most common cause of pneumonia is a pneumococcal infection caused by a bacteria called Streptococcus pneumoniae. As pneumonia can be life threatening, people at high risk of pneumonia may be offered a vaccine against the pneumococcal bacteria.
Influenza more commonly known as flu, is an illness caused by a virus that affects the whole body and often causes respiratory problems such as a sore throat or cough. It usually attacks the upper respiratory tract which involves the nose and throat and causes inflammation in these areas. It may also however affect the bronchi and the lungs itself which may cause breathing difficulties or lead to pneumonia. In the UK people who are particularly vulnerable to infection can be given the flu vaccine which may reduce symptoms. Antibiotics will not help to treat a viral infection.
COVID-19 is a viral infection caused by SARS-CoV-2 corona virus. It causes asymptomatic, mild to severe symptoms. The symptoms include fever, cough, loss of smell or taste, fatigue, short of breath, diarrhoea or more. In severe cases it can cause multi organ failure, septic shock, thrombo-embolism and death. Some people may have long term complications often referred to as long Covid. In the UK, vaccines and antivirals are available to prevent and manage the infection.
Tuberculosis (TB) and nontuberculous mycobacteria (NTM) are chronic bacterial infections most commonly seen in patients with weakened immune systems (such as patients with HIV/AIDS). However, in the last 20 years TB cases have gradually increased, particularly among ethnic minority communities who are originally from places where TB is more common. The infections caused by mycobacteria develop slowly and can affect the whole of the body as well as the lungs. Treatment for TB requires long term antibiotics usually for 6 months. Symptoms usually include a cough, weight loss and night sweats. The BCG vaccine is used to help protect against TB. Currently it is only offered to those at high risk of TB such as health care workers and children living in areas with high rates of TB or those who have close family members from countries with a high TB rate.
Pleuritis often known as pleurisy is caused by inflammation of the lining of the lungs (pleura). It is particularly painful when taking deep breaths or coughing. It can occur with bacterial and viral infections as well as diseases such as pneumonia, TB or pulmonary emboli. It can also be caused by other inflammatory conditions such as rheumatoid arthritis and inflammatory bowel disease. Occasionally it may also be associated with lung cancers particularly mesothelioma. However, pleuritis can also occur spontaneously where the lungs become inflamed for no apparent reason. Treatment of pleurisy therefore depends on the underlying cause.
A pleural effusion is a collection of fluid in the pleural space (the lining of the lungs). This then compresses the underlying lung tissue affecting breathing and the function of the lungs. There are many causes including infections in the lungs such as pneumonia and TB. Cancer may also be a cause as well as other conditions such as rheumatoid arthritis and SLE ( systemic lupus erythematosus). Heart failure can also cause a pleural effusion by causing increased pressure in the blood vessels in the lungs that may cause fluid to leak out into the pleural space. A low level of protein in the blood can also cause blood to seep out from the blood vessels into the lung tissue. Low levels of protein are often found in people with liver diseases such as cirrhosis, so liver disease can also cause a pleural effusion. A pleural effusion is usually confirmed on a chest X ray. In most cases the doctors will insert a chest drain to drain the fluid from the lungs if there is a large amount of fluid present. A sample of the fluid is then sent to the laboratory for analysis and can help doctors to find out what caused the fluid accumulation.
Lung cancer is the uncontrolled growth of cells in the lungs. The main risk for developing lung cancer is smoking. There are two main types, small cell and non-small cell lung cancers. Non-small cell cancer is the most common type and accounts for about 87% of all cases. It is divided into 3 types of cancer: adenocarcinoma, squamous cell carcinoma and large cell carcinoma. Squamous cell carcinoma is the most common form of non-small cell carcinoma and is usually caused by smoking. Small cell lung cancer is usually always caused by smoking also. Other cancers may spread to the lungs and are described as metastatic, because the cancer cells do not come from lung tissue originally. Mesothelioma is another type of lung cancer that develops in the pleura (the lining of the lung). This is usually caused by exposure to asbestos. Symptoms of lung cancer include coughing up sputum with small amounts of blood, a long term cough which doesn’t go away, unexplained weight loss and worsening shortness of breath.
A pulmonary embolism is a blockage in the pulmonary artery which is a blood vessel that carries blood from the heart to the lungs. This is normally caused by a blood clot that originated in the veins of the legs (also known as a deep vein thrombosis or DVT) but travelled up through the blood vessels and got stuck in the lungs. Pulmonary embolisms cause chest pain (which is usually worse on breathing in), sudden shortness of breath, and coughing (sometimes of blood). This condition can be life-threatening and requires urgent medical attention. Treatment is usually to thin the blood to stop the clot getting bigger whilst the body breaks down the original clot.
Pulmonary fibrosis is a disease with damage and scarring to the tissues between the air sacs, inflammation of the air sacs, and stiffening of the lungs. This impairs the elasticity of the lungs so that the lungs cannot expand and contract as well during normal breathing so that air cannot flow into and out of the lungs as easily. As the air sacs are also damaged gaseous exchange cannot occur as well as it normally does. Therefore this may cause shortness of breath, a lack of oxygen in the blood which may cause cyanosis (where the lips may turn blue) and a chronic cough. Pulmonary fibrosis is usually diagnosed on a chest X ray or CT scan of the chest and has many causes. Causes of pulmonary fibrosis include:
- Exposure to small particles (often at work). This includes repeated exposure to substances such as asbestos, coal, beryllium, and silica
- Repeated exposure to organic substances such as mouldy hay, animal droppings, and grain dust. This can cause an allergic inflammation pneumonitis) and eventually lead to pulmonary fibrosis
- Chemicals and drugs that are toxic to the lungs e.g. amiodarone, methotrexate.
- Previous radiation treatment
- Sarcoidosis and other granulomatous diseases.
- Systemic sclerosis, other autoimmune disorders and connective tissue disease such as SLE and rheumatoid arthritis.
- Inherited causes – e.g. neurofibromatosis, tuberous sclerosis, familial idiopathic pulmonary fibrosis.
- Other illnesses, including hepatitis C, inflammatory bowel disease, acquired immunodeficiency syndrome.
- Idiopathic – cause unknown. This is the most common cause.
Pulmonary hypertension is a rare lung disorder. This is caused by increased pressure within the pulmonary artery which is a blood vessel that transports blood from the right side of the heart to the lung to collect oxygen, This increase in pressure means the heart has to work harder to transport blood into the lungs. This can in turn cause damage to the heart, as the heart may become weaker from this increased work load and cause heart failure. Pulmonary hypertension can occur by itself but often happens with other problems such as heart and lung disease. It may also occur with pulmonary emboli and rare conditions such as systemic sclerosis which thickens and stiffens the walls of the pulmonary artery.
Bronchopulmonary dysplasia (BPD) is a lung disease that develops mainly in premature babies who have had long-term oxygen and/or been on a ventilator. It may also be seen in those who have experienced oxygen toxicity or had pneumonia such as term babies who have required aggressive ventilation for lung disease. With this disorder airways are inflamed, do not develop normally, and may be damaged.
Respiratory Distress Syndrome (RDS) of the newborn is a life-threatening breathing problem that may develop in babies born before 34 weeks. These premature babies’ lungs are not developed enough to be able to produce much of the protective liquid called surfactant. Without surfactant, the lungs are not able to expand properly and babies have difficulty breathing in enough oxygen. It can occur within a few hours of premature birth.
Acute Respiratory Distress Syndrome (ARDS) is a rapid, severe breathing difficulty due to extensive lung inflammation and the lungs filling with fluid. ARDS can be fatal and may be brought on by many types of injury to the lungs including serious viral or bacterial infection, sepsis, trauma, multiple transfusions, drug overdose, or inhaling substances such as salt water or smoke.
Cystic fibrosis is an inherited disease that affects the lungs, pancreas, and other body systems such as liver, nose, reproductive organs and sweat glands. This is due to a defect in a gene which causes sticky mucus to build up in the lungs and digestive system. In the lungs this thick sticky mucus can trap bacteria in the small airways leading to frequent chest infections and a productive cough. . Diarrhoea and low weight are due to pancreatic problems preventing absorption of nutrients. Cystic fibrosis commonly causes infertility in men. 1 in 25 people in the UK have 1 cystic fibrosis gene, but the disease doesn’t occur unless both parents pass the gene onto a child. According to the Cystic Fibrosis Trust 5 babies are born with cystic fibrosis in the UK each week.
Bronchiectasis is a condition where the airways of the lungs become abnormally enlarged. This causes a build- up of mucus in the airways which causes a chronic cough and can trap bacteria predisposing to infections. Treatment includes regular physiotherapy to help bring up the extra mucus and courses of antibiotics to treat any infection.
Alpha-1 antitrypsin deficiency is an inherited lack of a protein that provides protection to the lungs. This protein is produced in the liver. However in the alpha-1 antitrypsin deficient patient there is a problem with the structure of the chemical so that it cannot leave the liver into the blood stream to get to the rest of the body. Without this protection the lungs slowly become damaged and the elastic walls of the lung can be broken down. This puts the patient at an increased risk of COPD especially if they also smoke. In addition, the build-up of the protein in the liver can cause liver disease at a young age.
Other disorders do not affect the lungs directly, but can impair a person’s ability to breathe properly. These disorders may affect the chest cavity, muscles, nerves, and heart. They include a variety of conditions, such as nerve and muscle (neuromuscular) diseases like muscular dystrophy, polio, myasthenia gravis, Guillain-Barré syndrome, and amyotrophic lateral sclerosis (ALS, or Lou Gehrig's disease). Bony problems that result in abnormal spine formation or rib cage movement can restrict lung expansion. [Note: specific testing and treatment for these disorders is not covered in this article.]