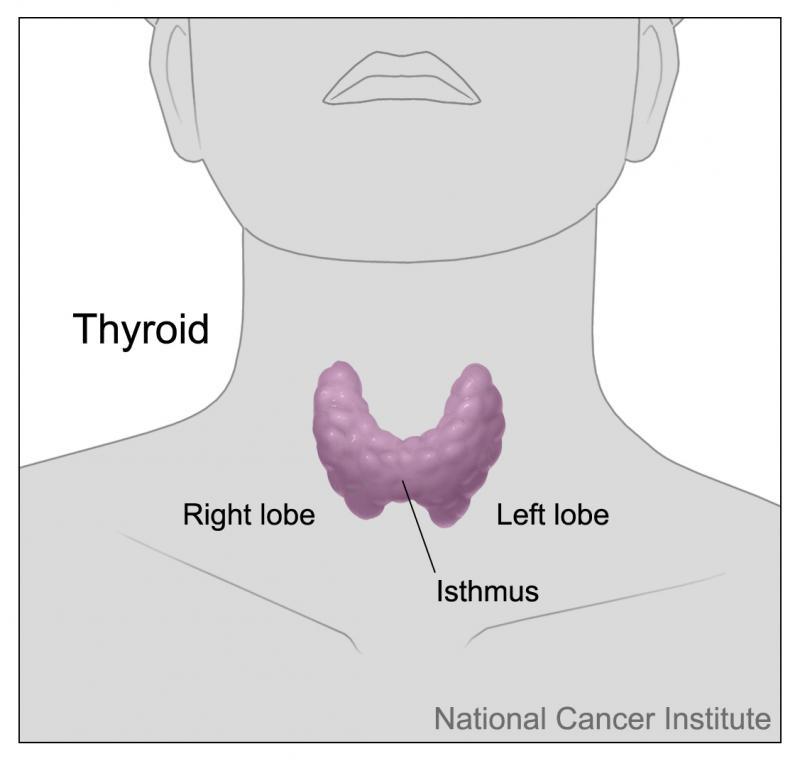
Hyperthyroidism - Hyperthyroidism means you have too much thyroid hormone. This makes your body use energy faster than it should and therefore some cells and tissues in your body work faster than they should do. of hyperthyroidism are:
- Palpitations (fast or abnormal heart rate)
- Feeling anxious, nervous, irritable or emotional
- Anxiety & depression
- Difficulty sleeping
- Diarrhoea
- Feeling hot
- Weakness & fatigue
- Weight loss despite feeling hungry
- Tremor
- Hair loss
- Light or absent periods
- A swelling of your thyroid gland ( goitre)
- Eye problems such as blurred vision and eyes that appear enlarged if you have a type of hyperthyroidism called Graves disease
It is important to realise that most people will not have all the symptoms and in some people the symptoms may be very mild at first.
Graves disease
Hyperthyroidism (the overproduction of thyroid hormone) can be caused by different mechanisms. Graves’ disease is the most common cause of hyperthyroidism. In Graves’ disease the body produces antibodies that damage the thyroid and cause the release of thyroid hormones. are produced to fight infections and any other harmful invaders that could damage the body. Sometimes, for reasons that aren't clear, the body produces antibodies that attack our own tissues. The production of antibodies against our own tissues leads to an autoimmune disease. In Graves’ disease, the thyroid gland, may become enlarged and swollen. An enlarged thyroid gland is called a goitre. These antibodies may also attack the eyes causing inflammation of the eye muscles. This can lead to problems with vision and also an enlargement of the eyes as the muscle behind the eyes becomes swollen.
Other causes of hyperthyroidism
Other causes of hyperthyroidism include inflammation of the thyroid gland which is known as thyroiditis. It generally occurs after a illness (which is known as subacute thyroiditis) or after a pregnancy (postpartum thyroiditis). Hyperthyroidism may also be caused by autoimmune diseases that are different to Graves disease, as well as by some medications e.g. amiodorone or lithium.
Less commonly hyperthyroidism is caused by a growth of part of the thyroid gland called a nodule. A nodule is simply a lump of tissue. One nodule may develop (e.g. toxic solitary adenoma) or occasionally multiple nodules may form (e.g. multinodular goitre).These nodules contain abnormal thyroid tissue so that the thyroid gland ends up producing more thyroid hormone than normal. They are usually non cancerous.
Treatment for hyperthyroidism
Treatment for hyperthyroidism often depends on the cause. However, options include having a single dose of radioactive iodine by mouth or by injection which gets taken up by the thyroid and kills some of the over productive cells. Other options include taking anti-thyroid tablets regularly (e.g. carbimazole) which suppresses the production of the thyroid hormone. These are usually taken for 1-2 years after which case the cause of the hyperthyroidism has normally resolved so the treatment can often be stopped. However a certain percentage of people may need to take carbimazole for the long term in order to keep their symptoms under control. Surgery to remove part of the thyroid is also an option and is often used in people with goitres that are large enought to put pressure on other areas such as the windpipe.
Occasionally some of these treatments may inadvertently stop too much of the thyroid gland from producing the thyroid hormones. This may then result in hypothyroidism and it may then be necessary to take thyroxine tablets to increase the thyroid hormone levels back to normal.
Hypothyroidism - Hypothyroidism means you have too little thyroid hormone. This makes your body use energy more slowly than it should and some parts of your body may work slower than normal. Hypothyroidism is common; in fact, you can have hypothyroidism for a number of years before it is recognised and treated. It is more common in women than men and it becomes more common as you get older. Symptoms of hypothyroidism include:
- Weight gain or fluid retention
- Depression
- Constipation
- Feeling cold
- Dry skin
- Thinning hair and brittle nails
- Tiredness
- Memory problems and poor concentration
- A slow heart rate
- Heavy /abnormal periods or infertility (not as common)
- Goitre (depending on the cause of the hypothyroidism)
Once again, sometimes only a few of these symptoms may be apparent in cases of hypothyroidism and the symptoms can often be mild.
Causes of Hypothyroidism
Hypothyroidism also has many different causes. Worldwide the most common cause is iodine deficiency as iodine is needed to make the thyroid hormones. However in the UK this is rare as our diet usually contains sufficient iodine. Vegetarians may have low iodine intake in their diet.
The commonest cause for hypothyroidism in the UK is an autoimmune disease called autoimmune thyroiditis. In this disease the thyroid gland is attacked by and can no longer make enough thyroxine. Hashimoto’s disease is the commonest form of autoimmune thyroiditis. In this form the thyroid gland also swells up and it is therefore associated with a goitre (swelling of the thyroid gland). Other rarer forms of autoimmune thyroiditis cause hypothyroidism.
Hypothyroidism may also occur secondary to treatment for an overactive thyroid (especially after surgery or radioactive treatment). In these cases too much of the thyroid tissue may have been damaged or removed and therefore the gland will not produce enough hormone. Medication (such as amiodarone or lithium) may also cause hypothyroidism by a variety of mechanisms In addition some children may be born with hypothyroidism if their thyroid gland has not developed properly. This is called congenital hypothyroidism. All babies are tested for this disease when they are born. Very rarely a problem with the pituitary gland in the brain may cause hypothyroidism. This is due to a lack of production from the pituitary of TSH so that the thyroid gets no signal to produce thyroid hormones when they are low. This is called ‘secondary hypothyroidism’.
Treatment for hypothyroidism is usually straightforward and involves taking tablets of thyroid hormone regularly. Treatment is usually life long as the condition is normally permanent.
Other Thyroid Diseases
Thyroid Cancer—There are 5 main types of thyroid cancer: papillary, follicular, medullary, anaplastic and thyroid lymphoma. Papillary and follicular cancers are slow growing and are usually straightforward to treat. Medullary cancer usually has a good outcome if it has not spread beyond the thyroid gland. Anaplastic thyroid cancer is the least common but it is the most aggressive form and spreads quickly. It can be difficult to treat. Lymphomas of the thyroid are not very common but are usually highly curable. Thyroid cancer may require different treatments such as surgery, chemotherapy, and radiotherapy depending on the type and how far the cancer has spread.
Solitary Thyroid Nodule—A solitary thyroid nodule is a small lump on the thyroid gland. By age 50 as many as 50% of the population will have a nodule somewhere in the thyroid. The overwhelming majority of these nodules are harmless. Some patients will have normal thyroid hormone levels. However some patients can have high or low thyroid hormone levels because of the nodules. Occasionally, thyroid nodules can be cancerous and need to be treated.
Goitre—A thyroid goitre is a visible enlargement of the thyroid gland. This rarely happens in developed countries, but is common in some areas in developing countries where there is little iodine in the diet. Iodine is needed to produce thyroid hormones so if iodineis in short supply the thyroid tries to compensate and grows in size. Other causes of a goitre involve an inflammation of the thyroid gland as occurs in Graves disease and Hashimoto's disease. Therefore goitres may be associated with producing too much or too little thyroid hormone. Sometimes however a patient with a goitre will have normal levels of thyroid hormones. Goitres can compress other structures of the neck such as the windpipe (trachea) and food pipe (oesophagus). This compression makes it difficult to breathe and swallow. The goitre has to be surgically removed.
Thyroiditis—Thyroiditis means that the thyroid gland is inflamed. This is usually due to autoimmune disease where the body produces antibodies that attack the thyroid gland. It may be also be due to a bacteria or a virus which act in the same was as antibodies in auto-immune disease to attack the thyroid gland. It can also occur after a pregnancy. Thyroiditis can cause hypothyroidism or hyperthyroidism and the symptoms can therefore vary. It can also cause fever and pain in the thyroid gland depending on the cause.What tests are used to detect a problem with the thyroid?