A common cause of hepatitis is an infection with a . The five viruses primarily associated with hepatitis are named in the order of their discovery: A, B, C, D, and E. In the UK, viral hepatitis is most commonly caused by hepatitis A (HAV), hepatitis B (HBV), and hepatitis C (HCV), while only HBV and HCV cause hepatitis.
Hepatitis A is spread through water and food that have been contaminated with the virus derived from human faeces and urine. Rates of hepatitis A have been dropping and are the lowest in 40 years due to a introduced in 1995. Hepatitis A causes an acute infection but not a chronic form of the disease. Treatment usually involves only supportive therapy, and most patients recover fully within about six months. Persons who have been in recent close contact with a known case of hepatitis A can benefit from prompt administration of prophylactic hepatitis A vaccine or human normal immunoglobulin.
Hepatitis B (HBV) can be spread by exposure to contaminated blood or needles, through unprotected sex with an infected person, and from an infected mother to baby. It is the most common cause of acute viral hepatitis. All pregnant women in the UK are offered hepatitis B screening and newborns of infected mothers areroutinely vaccinated which dramatically reduces the risk of them becoming infected.
Most adults with HBV will get better without any intervention, but about 1-3% become - chronically infected and able to spread the disease to others. Up to 90% of newborns and 25-50% of children 1 to 5 years old who are infected with hepatitis B virus develop a chronic infection. With the advent of screening pregnant women for hepatitis B and the vaccination of newborns, the number of infected babies has fallen. Most chronic hepatitis B infections are now seen in people born in parts of the world (particularly southern and eastern Asia, southern Europe, and Africa) where infection among newborns still remains common. An estimated 350 million people around the world are chronically infected with HBV.
Hepatitis C (HCV) is spread by exposure to contaminated blood. The most common mechanism of exposure is the sharing of needles or other "works" used in injecting drugs of abuse such as cocaine or heroin. Other means of becoming infected include occupational exposure of health care workers to used needles or other sharp objects, through sexual activity that results in tissue tears, from mother to baby during childbirth, and sharing personal items contaminated with blood such as razors and toothbrushes.
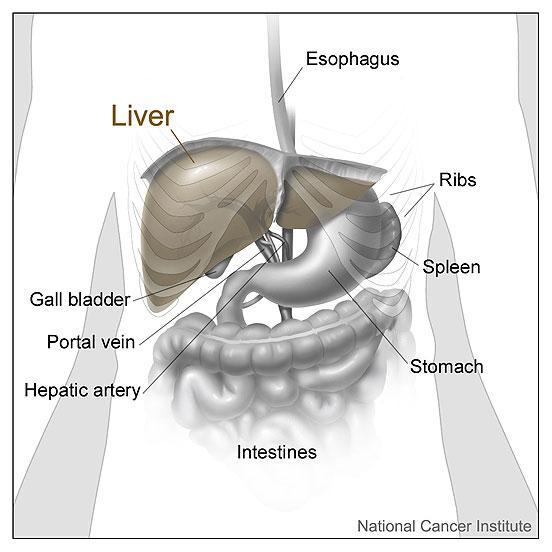
HCV is less common than hepatitis B as a cause of acute hepatitis but is the most common cause of chronic hepatitis. About 75% to 85% of those exposed to the virus develop chronic hepatitis C infection. In addition, about 60% to 70% develop chronic liver disease, roughly 5% to 20% will develop cirrhosis over many years, and 1% to 5% are estimated to die from a condition that results from chronic infection such as cirrhosis and liver cancer.
There is no vaccine available to prevent hepatitis C, but research is in progress to develop one. Currently, the best way to avoid getting infected is to limit exposure to possible sources of the virus, especially avoiding the sharing of needles to inject drugs.
Hepatitis D and E are rare. Hepatitis D only causes an infection when hepatitis B is present and can make that infection more severe. It is usually spread by exposure to blood or infected needles. Hepatitis E is spread in a similar fashion to hepatitis A and is found primarily in Asia, Africa, and South America.
Signs and Symptoms of viral hepatitis correspond to those of hepatitis in general. See the section on Signs and Symptoms for detailed information.
Laboratory Tests
There are a variety of antibody and antigen tests that are available to help diagnose and/or monitor hepatitis caused by the specific hepatitis viruses. For testing information on the most common causes of viral hepatitis, see the pages on hepatitis A, B, and C or see the summary information on them in the table below.
Summary Table: Most common causes of viral hepatitis
| Virus |
Hepatitis A |
Hepatitis B |
Hepatitis C |
| Transmission Route |
Faecal-oral |
Infected needle or blood, sexual contact |
Infected needle or blood, sexual contact |
| Incubation Time (acute infection) |
15-50 days |
45-160 days |
14-180 days |
| Onset |
Sudden |
Either sudden or slow, unnoticed |
Usually slow, unnoticed |
| Severity |
Mild |
Occasionally severe |
Usually slow-developing and symptoms not specific or strong |
| Chronic form? |
No |
Yes |
Yes |
| Associated with other diseases? |
None |
Liver cancer, cirrhosis |
Liver cancer, cirrhosis |
| Testing to Diagnose Acute Infection |
HAV-Ab, IgM |
HBsAg, Anti-HBc, IgM |
Anti-HCV, HCV RNA (note - may have same results as in chronic hepatitis) |
| Testing to Diagnose Chronic Infection or to Monitor Treatment |
N/A |
HBsAg, HBV DNA, HBeAg, Anti-HBe |
Anti-HCV (once), HCV RNA or viral load, HCV genotype (once) |
| Tests that Detect Previous Infection |
HAV-Ab, IgG |
Anti-HBs, Anti-HBc total |
Anti-HCV |
| Vaccine available? |
Yes |
Yes |
No |
| Common Treatment |
None |
Chronic form - Interferon, entecavir, tenofovir, lamivudine, adefovir |
Chronic form - Interferon (usually with ribavirin) |
|
Abbreviations Defined
HAV-Ab = Hepatitis A antibody
Anti-HBs = Hepatitis B surface antibody
HBsAg = Hepatitis B surface antigen
HBeAg = Hepatitis B e-antigen
Anti-HBe = Hepatitis B e-antibody
Anti-HBc = Anti-hepatitis B core antigen
HBV DNA = Hepatitis B Virus DNA (test for virus genetic material)
Anti-HCV = Hepatitis C antibody
HCV RNA = Hepatitis C Virus RNA (test for virus genetic material)
HCV Viral Load = A detection and/or count of the amount of virus in the blood
HCV Genotype = Determines the type of Hepatitis C present (1 of 6 types)
|
Prevention
The incidence of new cases of viral hepatitis has decreased due to use of safe injection and safe sex practices (important in preventing hepatitis B and C) and the availability of vaccines for hepatitis A and hepatitis B (there is currently no vaccine available for hepatitis C). Screening units of blood for hepatitis B and C has virtually eliminated infections through blood transfusions. A systematic programme to screen pregnant mothers for hepatitis B and to vaccinate all newborns with infected mothers has greatly decreased new cases of hepatitis B.
Treatment
Support and symptom relief are frequently the only treatments required for acute viral hepatitis A, B, and C. This usually involves plenty of rest, fluids, and nutritious food. With hepatitis A, most people recover without any complications. With hepatitis B and C, some people may develop chronic forms of the disease. The goal with chronic forms is to minimise further damage to the liver, to treat underlying conditions that are causing or exacerbating the condition, and to prevent transmission of viral hepatitis to others. There are medications available to treat chronic hepatitis B and C, but not all people need to be treated. The antiviral drugs that are given can have serious side effects. Often, people with chronic hepatitis will be closely monitored to see if they develop cirrhosis or liver cancer. New treatments, vaccines, and prevention strategies for viral hepatitis continue to emerge. It is important to talk to your doctor about the risks and benefits of currently available options.