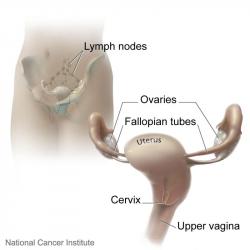
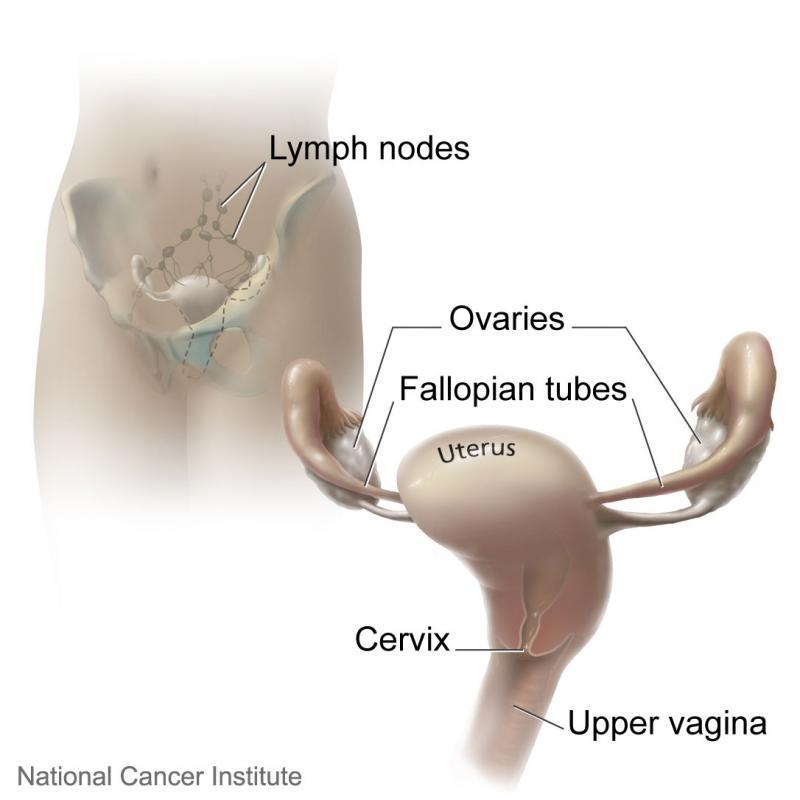
Pelvic inflammatory disease (PID) is an inflammation and infection of a woman’s upper reproductive organs. It occurs when bacteria move from the vagina, upward through a layer of mucus that protects the opening of the cervix, and into the uterus, fallopian tubes, and ovaries. PID can cause an acute illness, chronic pain, or it may be present as an almost silent long-term infection. Left untreated, it can cause scarring and irreversible damage to one or more of the reproductive organs. Scarring in the fallopian tubes can cause infertility and significantly increase the risk of an ectopic pregnancy.
Pelvic inflammatory disease is primarily associated with Chlamydia trachomatis and Neisseria gonorrhoeae, two common microorganisms that cause the sexually transmitted diseases (STDs) chlamydia and gonorrhoea. PID may also be caused by bacteria typically found in the vagina or gastrointestinal tract - such as Gardnerella vaginalis or Escherichia coli, and by a variety of other pathogens.
Although PID can affect any woman at any age, with or without sexual transmission, most cases occur in sexually active women of childbearing age. Those at increased risk include women who began having sex at a young age, those with multiple sexual partners, a new partner, those with the recent instrumentation of the uterus and those who have had a previous STD or PID. A woman with an intrauterine device (IUD) may be at an increased risk for a few months after its insertion. Douching may increase the risk of PID because the practice can change the vaginal normal flora and can potentially flush bacteria into the uterus. Since the uterus is sealed off during gestation, an occurrence of PID during pregnancy is rare.