To help diagnose or rule out a phaeochromocytoma or other neuroendocrine tumour
Catecholamines, plasma and urine
If you have symptoms of persistent or episodic high blood pressure such as severe headaches, rapid heart rate and sweating
A 24-hour urine sample (collected into a bottle containing a small amount of acid) or possibly a blood sample taken from a vein in the arm
Note: These tests are affected by certain drugs, foods, and stresses. Inform your doctor of any medicines you are taking and follow any instructions you are given for things to do or foods to avoid before sample collection.
No preparation is required before collecting a urine sample.
For a blood sample you may be asked to lie down and rest quietly for 15-30 minutes prior to sample collection, and your blood may be collected while you are lying down. In other circumstances, you may just be seated upright with little or no rest time before the sample collection.
-
How is it used?
Catecholamine testing is mainly used to help detect and rule out phaeochromocytomas in patients with symptoms. It may also be used to help monitor the effectiveness of treatment when a phaeochromocytoma is discovered and removed and to look for recurrence. The blood test is most useful when a patient has persistent high blood pressure or whilst experiencing an episode of hypertension. It is important to measure the hormone when a patient has symptoms because the hormones do not linger in the blood; they are used by the body, metabolised, and removed in the urine. Urine catecholamine testing measures the total amount of catecholamines released over a 24 hour period. Since the hormone levels may vary during the day, the urine test may detect excess production that is missed with the blood test. You may be asked to collect more than one urine sample; this increases the chances of including an episode of increased catecholamine production.
The doctor may use a combination of urine catecholamines, plasma catecholamines, urine metadrenalines and plasma metadrenalines to look for very high levels of catecholamines and their metabolites.
Since these tests are can be affected by drugs, foods, and stresses, there will be a certain number of false positives. For this reason, catecholamine testing is not recommended as a screen for the general public. Doctors will frequently investigate a positive result by looking at a patient’s stresses, food and drug intake, then work to reduce any influences, and repeat the test to see whether the change(s) have been effective.
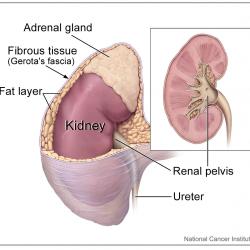
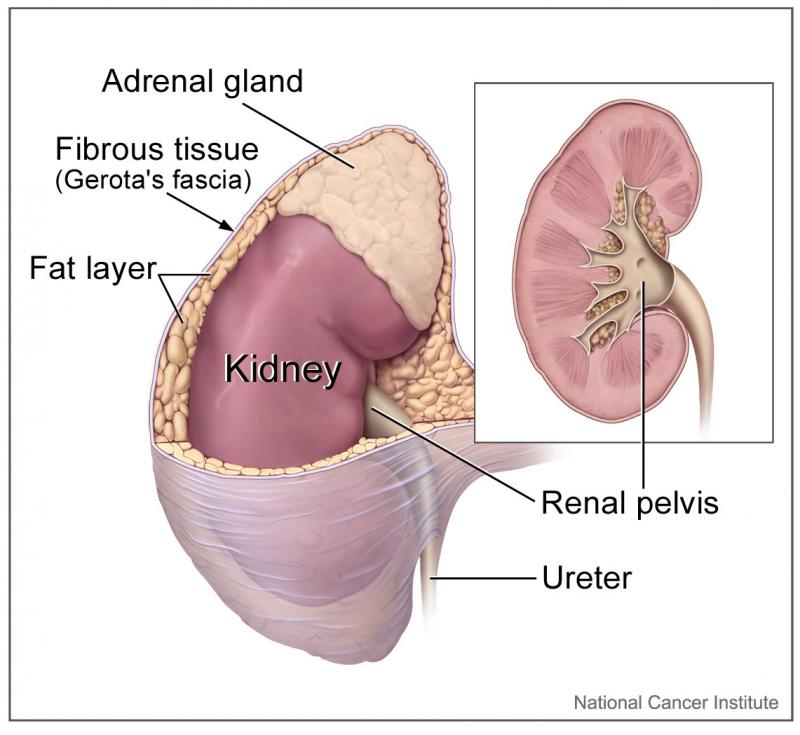
Occasionally, the tests may be used on an asymptomatic person if an adrenal or neuroendocrine tumour is found on a scan that is done for another purpose or if the patient has a strong personal or family history of phaeochromocytoma (as they may recur and there is a genetic link in some cases).
-
When is it requested?
Catecholamine testing is used when a doctor either suspects that a patient has a phaeochromocytoma or wants to rule out the possibility. The doctor may request it when a patient has persistent or recurring high blood pressure with symptoms such as headaches, sweating, flushing, and rapid heart rate. It may also be requested when a patient has high blood pressure that does not respond to treatment (patients with a phaeochromocytoma are frequently resistant to normal drugs).
Occasionally, the test may be used when an adrenal tumour is found by accident following a scanning procedure (this is called an adrenal incidentaloma) or when a patient has a family history of phaeochromocytoma. It may also be used as a monitoring tool when a patient has been treated for a previous phaeochromocytoma.
-
What does the test result mean?
Since the measurement of catecholamines and their metabolites is sensitive to many outside influences and phaeochromocytomas are rare, a doctor may see more false positives with this test than true positives. If a symptomatic patient has large amounts of catecholamines and or catecholamine metabolites in their blood or urine, further investigation is indicated. Serious illnesses and stresses can cause moderate to large temporary increases in catecholamine levels. Doctors must evaluate the patient as a whole - his or her physical condition, emotional state, medicines, and diet. When interfering substances or conditions are found and resolved, the doctor will frequently re-test the patient to determine whether the catecholamine and catecholamine metabolites are still high. The doctor may also request imaging tests (such as an MRI scan) to help find any tumour.
If levels are elevated in a patient who has had a previous phaeochromocytoma, then it is likely that either treatment was not fully effective or that the tumour is recurring.
If the concentrations of catecholamine and catecholamine metabolites are normal in both the plasma and urine, then it is unlikely that a patient has a phaeochromocytoma. Phaeochromocytomas do not necessarily produce catecholamines at a constant rate. However if the patient has not had a recent episode of hypertension, their plasma and urine concentrations of catecholamines could be at normal or near normal levels even when a phaeochromocytoma is present. Under these circumstances the measurement of urine and plasma catecholamine metabolites is helpful as they are continually produced by the tumour and therefore may be elevated when urine and plasma catecholamines are normal.
-
Is there anything else I should know?
While plasma and urine catecholamine testing can help detect and diagnose phaeochromocytomas, they cannot tell the doctor where the tumour is, whether there is more than one, or whether or not the tumour is benign (although most are). The amount of catecholamines produced does not necessarily correspond to the size of the tumour. This is a physical characteristic of the tumour tissue. The total amount of catecholamines produced will tend to increase, however, as the tumour increases in size. It is very important to talk to your doctor before discontinuing any prescribed drugs. The doctor will work with you to identify interfering substances and drug treatments to find out which of them can be safely interrupted and which must be continued for your well-being.
Some of the substances that can interfere with catecholamine testing include: ACE inhibitors, paracetamol (acetaminophen), adrenaline, ethanol (alcohol), aminophylline, amphetamines, appetite suppressants, coffee, tea, and other forms of caffeine, chloral hydrate, clonidine, dexamethasone, diuretics, insulin, imipramine, lithium, methyldopa, MAO (monoamine oxidase) inhibitors, , nicotine, nitroglycerin, propafenone, reserpine, aspirin (salicylates), theophylline, tetracycline, tricyclic antidepressants, and vasodilators.
The effects of these drugs on catecholamine results will be different from patient to patient and are often not predictable. Bananas, pineapple and capsicums may also cause falsely elevated catecholamine results and should be avoided for 24 hours before and during the urine collection.
-
Is there any way to prevent a phaeochromocytoma from forming?
No, they can be detected and removed but not prevented. In most cases, the tumour is benign and, once it is removed, it will not recur.
-
Can I test for catecholamines at home?
-
Is it really necessary to collect urine for 24 hours?
-
Can my state of mind really affect my test results?