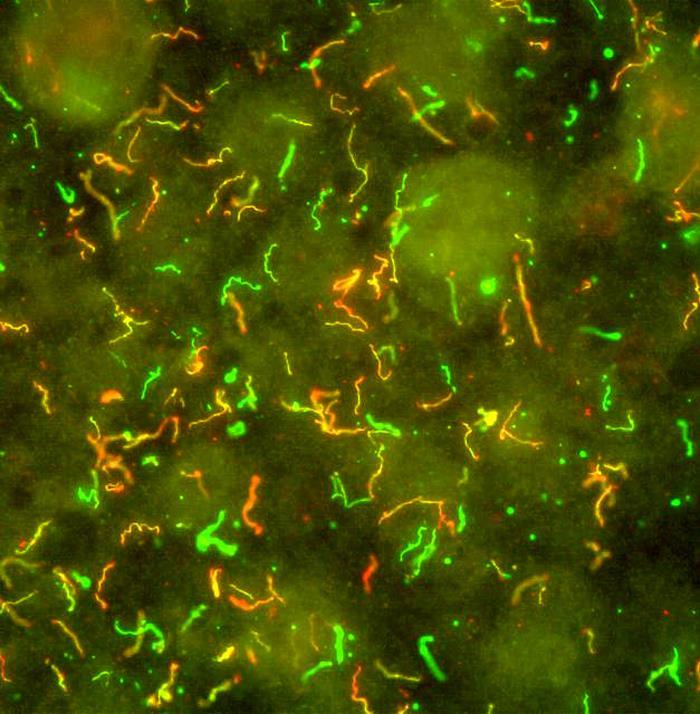
Lyme disease is an infection caused by a spiral bacterium, Borrelia burgdorferi, carried by a tick the size of the head of a pin. The tick is found in woods and heathland areas where it infests small animals and birds. People bitten by an infected tick which is not removed within a day or two may develop Lyme disease. An expanding rash called erythema migrans appears at the site of the bite within 3 to 30 days in a large proportion of those infected. Some develop flu-like symptoms with aching joints and muscles. The disease can later affect the nervous system, joints and other body systems.
The best defences against Lyme disease are wearing protective clothing, using an insect repellent, and checking for (and carefully removing) ticks at regular intervals. Tests that can help diagnose Lyme disease detect antibodies that the body develops against the Borrelia burgdorferi bacterium. They appear some weeks after being bitten, so the tests may be negative if done too early and may need to be repeated a few weeks later.