Lupus (SLE) is a chronic, inflammatory autoimmune disorder that may affect many organ systems including the skin, joints, blood cells and internal organs, especially kidneys, and sometimes the brain. SLE affects women nine times more often than men and it usually occurs between the ages of 20-40 years although children, including newborns, and older adults can also have lupus. There is an increased incidence of lupus in persons of African, and Asian descent. The cause of lupus is not fully understood. It is thought to involve both an inherited component and a trigger that may be related to environmental factors and/or to hormones. Certain drugs may also cause SLE.
Lupus may co-exist with other autoimmune disorders, such as Sjögren’s Syndrome, thyroid disease, and the antiphospholipid syndrome.
Systemic Lupus Erythematosus
-
Types
There are many types of lupus. Some of these are listed below.
- Systemic lupus erythematosus (SLE)--. It affects many parts of the body (systemic).
- Discoid lupus--this type is characterised by a chronic skin rash, such as on the face or scalp; about 15% to 20% of people with this condition will progress to SLE.
- Subacute cutaneous lupus--associated with skin lesions on parts of the body that are exposed to sunlight.
- Drug-induced lupus--a form of lupus that can be caused by certain medications, such as some anti-seizure, high blood pressure, and anti-thyroid medications. The most common medications known to cause drug-induced lupus are the antibiotic isoniazid (used to treat and prevent tuberculosis), hydralazine (used to treat hypertension or high blood pressure), and procainamide (used to treat abnormal heart rhythms). Symptoms tend to occur after taking the medication for several months and usually resolve once the medication is stopped.
- Neonatal lupus--a rare form of lupus that affects newborns and that is characterised by a skin rash, liver problems, and low blood counts at birth. These usually resolve over several months. Newborns who have neonatal lupus may be born to women who have SLE, Sjögren syndrome, or no particular disease, but it is thought that it may be triggered in part by certain autoantibodies in the mother's blood (anti-SSA and anti-SSB), which cross the placenta into the fetus's/infant's bloodstream and can persist for several months. Women known to have these autoantibodies may be monitored more closely during their pregnancy.
-
Signs and Symptoms
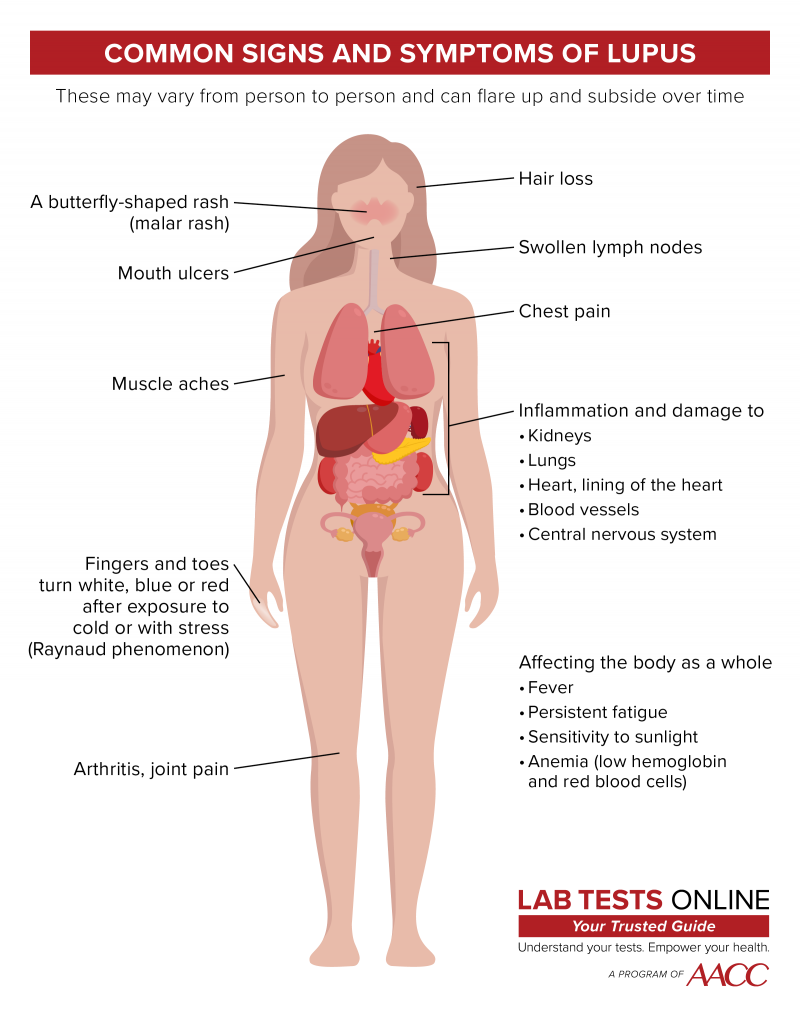
Signs and symptoms of lupus vary from person to person and by the type of lupus.
People with lupus may develop a rash, such as:
- A rash resembling a butterfly that appears across the nose and cheeks (malar rash)
- A red rash consisting of round or oval-shaped patches (discoid rash)
- A rash on areas of the skin that are exposed to sunlight (typically the face and extremities)
A rash is typically the only symptom in discoid and subacute cutaneous lupus. People with other types of lupus may have a combination of the following additional signs and symptoms:
- Muscle pain
- Arthritis-like pain in one or more joints (but no or little joint damage)
- Fever
- Persistent fatigue
- Swollen lymph nodes
- Sensitivity to sunlight
- Raynaud phenomenon (fingers change colour after exposure to cold temperatures or with stress)
- Hair loss
- Chest pain
- Anaemia
- Mouth ulcers
- Inflammation and damage to organs and tissues, including the kidneys, lungs, heart, lining of the heart, central nervous system, and blood vessels
- Kidney disease is a frequent occurrence in patients with lupus. Lupus causes glomerulonephritis, a condition that affects the kidney’s ability to filter toxins, which can lead to kidney failure if untreated.
- Sometimes involvement of the nervous system may occur and can lead to complications including headaches, seizures, depression, or even psychosis.
Symptoms of lupus may come and go over time and vary from person to person. They may worsen abruptly and then die down. Flare-ups may be triggered by changes in someone's health status, such as physical or emotional stressors, and/or by outside stimulants such as exposure to sunlight. Women may experience flare-ups during pregnancy or shortly after giving birth.
People with lupus are at increased risk of infections, such as urinary tract infections, respiratory infections, yeast infections, salmonella, herpes and shingles, due to their weakened immune system from both the condition and its treatments. They are also at increased risk of cancer, bone tissue death, and pregnancy complications, including miscarriage and pre-eclampsia.
Some patients with lupus may also be affected by the antiphospholipid syndrome, where the blood becomes more prone to clot: this can lead to clots in arteries leading to strokes, and in veins such as deep vein thrombosis in the legs, or pulmonary embolism (blood clot in the lung). The antiphospholipid syndrome also leads to an increased risk of miscarriages. Antiphospholipid syndrome can also occur in the absence of underlying lupus.
-
Tests
Diagnosis is made by, clinical evaluation of patient symptoms and examination findings, as well as the results of investigations. The following laboratory tests may be useful in the diagnosis of SLE:
- Anti-nuclear antibody test (ANA) is positive in almost all patients with SLE.
- Anti-double stranded DNA antibodies are frequently present, may be associated with kidney involvement and the level can fluctuate with disease activity making this a useful test to monitor.
- Anti-Sm (specific to lupus, but only seen in 10-30% of cases)
- Anti-SSA (Ro) and anti-SSB (La) antibodies may also be positive
- Antiphospholipid antibodies
- Additional rarer autoantibodies may be tested and be detected as part of diagnosis if there is a high clinical suspicion and many of the standard antibody tests above are negative.
- Testing for autoantibodies
- Urine analysis– may show blood, microscopic casts of kidney cells, or protein
- Full blood count (FBC) – decrease in some cell types, including white cells and platelets
- Serum protein electrophoresis – increased immunoglobulins
- Erythrocyte sedimentation rate (ESR) – increased
- C-reactive protein (CRP) is typically normal, unless coexistent infection is present
- Complement 4 (C-4) – may be decreased; the level can fluctuate with activity of the disease. Complement C3 may also be low, but more often with infection or severe flares of disease.
-
Treatment
There is currently no cure for lupus, although many patients may experience remissions of symptoms between flare-ups, often with the help of treatment. The goals of treatment are to alleviate symptoms, to minimise the occurrence of flare-ups and to minimise and address the development of complications associated with SLE. To help decrease the number of flare-ups, patients should get sufficient rest, maintain a degree of exercise, and should minimise stress and avoid exposure to ultraviolet light.
Patients should work closely with their doctor and with their specialist (often a rheumatologist, a specialist in joint disease) to develop a treatment plan that is effective for them. This plan is likely to change over time with changes in the patients’ symptoms, their general state of health and as new treatments become available. Women wanting to become pregnant should talk to their doctor about their health and their medications. Some treatments are safer than others for the developing infant during pregnancy.
The types of treatment that are used depend on what symptoms and complications the patient is experiencing at that time and their severity. Patients may take non-steroidal anti-inflammatory drugs (NSAIDs) to help alleviate pain and inflammation, though caution is needed if there is kidney disease. Antimalarial drugs such as hydroxychloroquine, and chloroquine may be given to help ease lupus skin and joint symptoms and to help inhibit flare-ups. For more severe symptoms, corticosteroids (such as prednisolone) and immunosuppressants (such as azathioprine, cyclophosphamide, mycophenolate mofetil or methotrexate) may be given - despite their associated side effects. It is important to discuss and assess the risks and benefits associated with these drugs with your healthcare professional before starting.
-
My doctor told me my ANA test is positive but is not sure I have lupus. How can this be?
The body’s immune system normally produces antibodies that are designed to fight off diseases and infections. In an autoimmune disease, something goes wrong with this system and the person’s body begins producing antibodies against their own tissues. Antinuclear antibodies (ANA) are antibodies that react with the cell nucleus (the central controlling part of the cell).
The ANA test looks at the concentration of antinuclear antibodies in a person’s blood. A positive result means that you have a higher than “normal” concentration of these antibodies. The incidence of a positive ANA in normal people increases with age, and for example, it is quite common to find a weak positive ANA in the elderly population, in whom lupus is rare. Weak positive ANAs are also more common in women, the majority of whom do not have SLE.
ANA testing is one of the tools in diagnosing lupus as well as several other autoimmune diseases, so a positive result may be related to lupus or another disease. Just having a positive ANA blood test does not equate to a diagnosis of lupus. You may simply have a higher than normal concentration of these antibodies. To make a diagnosis of lupus, there should be suggestive clinical features, and often other abnormal laboratory test results.
Even among people with lupus, the ANA results can vary widely – one person can be in remission at a certain level of ANA while another can be extremely ill at the same level. Interpreting what these results mean for you is the work of your doctor.
For more FAQs, see the ‘Lupus A to Z: Q & A Overview’ pages on the Lupus UK website.