A Novel, High-sensitivity, Bacteriophage-based Assay Identifies Low-level Mycobacterium tuberculosis Bacteremia in Immunocompetent Patients With Active and Incipient Tuberculosis
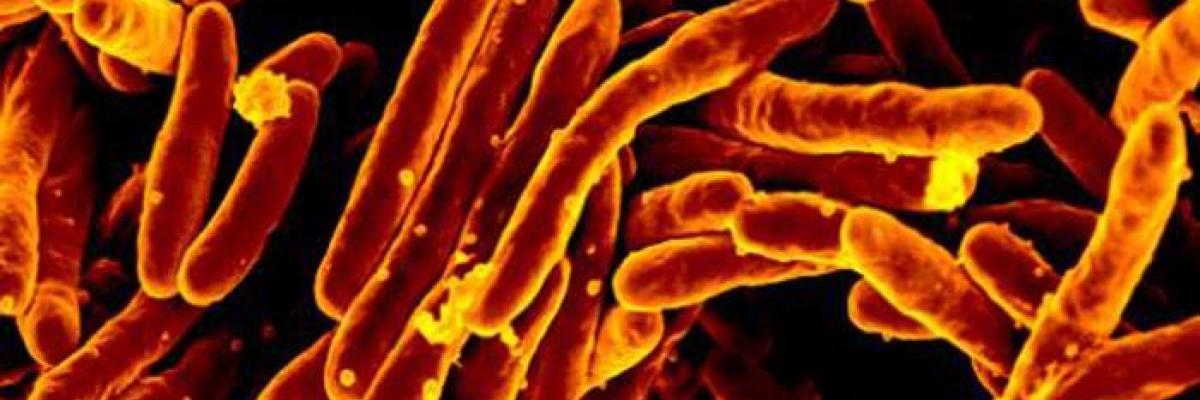
Tuberculosis (TB) is an infectious disease caused by bacteria of the Mycobacterium tuberculosis (MTB) complex. It remains the ninth leading cause of death worldwide, with an estimated 1.6 million deaths in 2017, and its epidemiology varies substantially around the globe, with the highest number of cases observed in sub-Saharan Africa, India and south-east Asia. In the UK, there have been annual declines in its incidence since 2011 and the main burden of disease is concentrated in large urban areas, with the highest proportion of cases in London, followed by Leicester, Birmingham, Luton, Manchester and Coventry. Despite such improvement, the diagnosis of TB is still problematic and culturing the bacterium can take up to several weeks. The traditional methods are generally based on prolonged cultures from respiratory samples or other tissue or body fluids. Some rapid diagnostic tests are available and they are based on the molecular amplification of genetic material (or DNA) of MTB. However, these methods are generally limited by the mycobacterial tough cell wall and they cannot be generally performed on blood samples due to undetectable levels of circulating DNA. More information about the disease and its diagnosis can be found on here.
Researchers from the universities of Leicester and Nottingham have recently published a new study on a blood test that has the potential of revolutionizing the diagnosis of TB. They have demonstrated that MTB is actually circulating in the blood at very low levels, despite the disease mostly involving the lungs. The novelty is that a specific bacteriophage has been used to increase the number of detectable bacteria in the blood. Bacteriophages are viruses that can infect bacteria but not humans. During the infection of bacteria, they generally cause the destruction (or lysis) of the bacteria and this significantly increases the release of DNA in the blood sample (plus the multiplication of the bacteriophage). This new Actiphage® technology has been developed by the University of Nottingham in collaboration with Royal Veterinary College and commercialised by PBD Biotech to be used in the detection of bovine TB. To conduct the test, the sample are incubated with the bacteriophage and the amplification can be monitored to produce specific result within 6-8 hours. The study is the first demonstration of a blood test for the diagnosis of active infection in humans.
For their first trial in humans, the researchers recruited 66 participants and divided them in four groups, including patients with active pulmonary TB, patients with latent TB infection, a first control group of 5 patients with other respiratory infection (non-TB) and a second control group of healthy individuals. This Actiphage® test was performed twice in all 66 participants, with an interval period of approximately 12 months. The results demonstrated a sensitivity of 73.3% and a specificity of 100%. There were 15 patients with active infection and the test was positive in 11 of them. More interestingly, two of the participants with latent infection (and no clinical or radiological evidence of infection) tested positive with Actiphage® test and they then developed active infection after some months. The authors explained that this could be due to a different immune response in different patients, with the test being able to detect the infection very early in those patients where the immune system may be failing to effectively contain the bacteria within the lungs.
The test was conducted on a small sample size and it is still early days before it can be implemented in routine clinical practice. Nevertheless, the preliminary results are very encouraging and this test has the potential to improve earlier diagnosis, in particular in patients unable to produce sputum samples. Further studies are needed to assess this new exciting technology.

